What is a Co-Occurring Disorder?
A person with co-occurring disorders has both a mental disorder and an alcohol or drug problem. These conditions occur together frequently. About half of people who have a mental disorder will also have a substance use disorder at some point in their lives and vice versa. The interactions of the two conditions can worsen both. [1]
Although these problems often occur together, this does not mean that one caused the other, even if one appeared first. In fact, it can be hard to figure out which came first. Researchers think that there are three possibilities as to why they occur together:
- Common risk factors may contribute to both mental disorders and substance use disorders. These factors include genetics, stress, and trauma.
- Mental disorders can contribute to drug use and substance use disorders. For example, people with mental disorders may use drugs or alcohol to try to feel better temporarily. This is known as self-medication. Also, mental disorders may change the brain to make it more likely you will become addicted.
- Substance use and addiction can contribute to the development of a mental disorder. Substance use may change the brain in ways that make you more likely to develop a mental disorder.

Symptoms
In Comparison to Mental Illnesses, Dependence on Heroin, Cocaine, Pain Medications, Marijuana, and Hallucinogenic Drugs Has Many Prominent Symptoms. [2]
- Euphoria
- Low hunger
- Depression
- Sleeping problems
- shaky hands and sweaty palms
- Excessive activity
- Vomiting and nausea
- An irregular heartbeat
- People’s personalities and attitudes suddenly shift
- Unsatisfactory performance at school or work
- Feeling down
- Fright
- Withdrawal from society
- Being forgetful
Bipolar Dysfunction, Grief, and Schizophrenia are Some of the Illnesses Which May Lead To:
- Depression
- Euphoria
- Social isolation
- Irritability
- Irrational or hallucinatory thoughts
- Suicidal tendencies
- Problems related to anger
- Anxiety and fear
Mental Illnesses, as Well as Addictive Disorders, are Also Associated with Similar Consequences. A Few are:
- Irreversible brain damage
- Relationships with unreliable partners
- Monetary difficulties
- Lay-off
- Poor health
- Suicide risk increases
Co-occurring disorders, such as depression, anxiety, and mental illness are more common in people with a family history of depression and anxiety. People with first-degree relatives are more likely to suffer from mental disorders such as despair, bipolar, anxiousness, and obsessive-compulsive dysfunction than anyone else, suggesting that these conditions may be inherited.
Common Co-Occurring Disorders
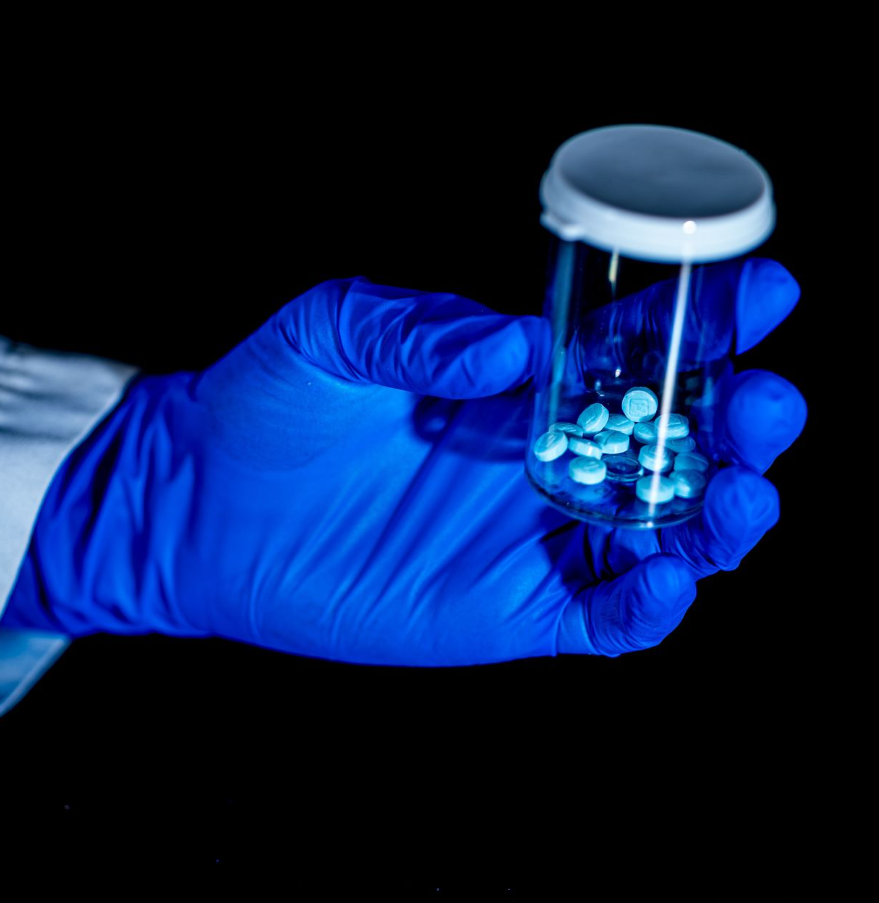
The misuse of pills and liquor can be caused by underlying mental health concerns, including loneliness, loneliness, and shame. People abuse these things to adapt to a broad variety of passions and activities, such as distress, stress, blame, and humiliation.
Abuse/Neglect
70-90% of child maltreatment involves some form of substance use.
Substance Use in Abuse and Neglect Cases
- Any history of substance abuse within a person’s
- lifetime is associated with increased risk of abuse/neglect
- Substance abuse is associated with up to 2/3 of child maltreatment fatalities
Addictions/Substance Abuse
As a country, we have a serious substance misuse problem — the use of alcohol, illegal drugs, and/or prescribed medications in ways that produce harm to ourselves and those around us. These harms are significant financially with total costs of more than $420 billion annually and more than $120 billion in healthcare. But these co-occurring disorders are not simply financial burdens — they deteriorate the quality of our health, educational, and social systems, and they are debilitating and killing us — particularly our young through alcohol-related car crashes, drug-related violence, and medication overdoses. [3]
Aging
Specific age-related factors can lead to substance use disorders or co-occurring disorders. Older adults are more likely to undergo traumatic experiences like bereavement. Many people struggle to cope with retirement. Loneliness following the loss of a spouse is common. Reduced mobility and the need to rely on others to carry out routine tasks can undermine self-confidence. Any of these can prompt people to turn to drugs or alcohol for relief.
Anxiety/Phobia
Many individuals with anxiety and mental illness turn to substance abuse for relief or to ease the burden every day. There are many types of anxiety and it is one of the most prevalent mental health disorders. In social situations, drinking can reduce anxiety, and prescription drugs can take away anxiety. As anxiety and mental illness sufferers consume substances to cope with their symptoms, their dependency on those substances increases, making them more vulnerable to addiction and making their anxiety worse. [4]

People with anxiety, phobias, or PTSD experience conditions such as traumatic brain injury (TBI) and PTSD more frequently than individuals who do not. Many veterans return from war with PTSD from their traumatizing combat experiences. The development of PTSD may be accompanied by psychological, physical, or sexual abuse.
Many different co-occurring disorders symptoms may indicate post-traumatic stress disorder, such as flashbacks, intrusive thoughts, horrors, and hyper-vigilance. Additionally, medications and liquor are temporary remedies for PTSD. The indications of PTSD may occur sooner, create more serious contradictory emotions, or interrupt sleep schedules. As PTSD symptoms can be debilitating, some victims lose control and abuse drugs or alcohol to cope.
Attention Deficit/Hyperactivity
It is now recognized that attention-deficit/hyperactivity disorder (ADHD) may persist into adulthood. A number of studies have found an association between ADHD and substance abuse. Attention-deficit/hyperactivity disorder (ADHD) is a mental health disorder that affects attention and self-control.
Like many mental illnesses, ADHD often co-exists alongside drug addiction (also called substance use disorder). This is called a dual diagnosis. It requires specialized co-occurring disorders treatment that addresses both ADHD and addiction.
Bipolar Disorder
Those who suffer from Bipolar disorders and mental illness experience excessive and unruly scenes of both sadness and obsession due to an imbalance in brain chemicals. The cruelty of these incidents is typically reduced through the abuse of drugs, which ultimately leads to increasingly irregular brain activity. Some studies suggest that bipolar depression and mental illness may be associated with substance abuse disorders when compared to conditions not diagnosed with bipolar disorder.
Depression/Mood
In many cases, people abuse substances to feel joy or pleasure, even if artificially, even if they need to become numb to their emotional pain. Depression is one of the most common mental illnesses across the globe, affecting millions of people worldwide. But substance-induced depression, also recognized as drug-induced happiness, also happens with alcohol and other drugs after the first elation has worn off. Substance abuse then increases, as the individual desires both euphoria and to avoid contradictory emotions. A bad series thus occurs where depression intensifies dependence and vice versa.
Dissociation
Specifically, substance use and dependence were among the most common diagnoses in patients with a dissociative identity disorder. Dissociative drugs can produce visual and auditory distortions and a sense of floating and dissociation (feeling detached from reality) in users.
Alcohol slows down cognitive processes and can provide temporary relief for people with overactive minds. However, it ultimately exacerbates dissociative symptoms. Not only does alcohol blunt sensations, but it can also induce dissociative amnesia through blackouts.
Eating Disorders
Eating disorders frequently co-occur with addiction, and stimulants are among the many substances people turn to when they are struggling with these devastating conditions. Stimulants include illicit drugs such as cocaine and methamphetamines and prescription medications such as Adderall and Ritalin.
Obsessive-Compulsive Spectrum Disorders
Obsessive-compulsive spectrum disorders are a group of similar psychiatric disorders characterized by repetitive thoughts, distressing emotions, and compulsive behaviors. The specific types of thoughts, emotions, and behaviors vary according to each disorder.
Personality Disorders
BPD or borderline personality disorder is a mental illness characterized by sudden mood swings, extreme temperamental restlessness, unpredictable behavior, scattered thoughts of self, others, and the environment, and trouble forming steady connections. Around 6% of adults in America suffer from this disorder. People who suffer from these symptoms often abuse drugs and alcohol to adapt to “controllable” symptoms. This temporary relief is usually short-lived, and can sometimes aggravate symptoms of mental illness. [5]

Psychosis/Schizophrenia Spectrum Disorders
Doctors who specialize in mental health used to divide schizophrenia into different subtypes: Catatonic. Disorganized. Paranoid. Up to 50% of patients with schizophrenia exhibit either alcohol or illicit drug dependence, and more than 70% are nicotine-dependent. In particular, heavy cannabis abuse has been reported to be a stressor, eliciting relapse in patients with schizophrenia and related disorders. [d]
Sleep Disorders
Most common mental disorders, from depression and anxiety to PTSD, are associated with disturbed sleep, and substance use disorders are no exception. The co-occurring disorders relationship may be complex and bidirectional: Substance use causes sleep problems, but insomnia and insufficient sleep may also be a factor raising the risk of drug use and addiction. Recognizing the importance of this once-overlooked factor, addiction researchers are paying increased attention to sleep and sleep disturbances, and even thinking about ways to target sleep disruption in substance use disorder treatment and prevention.
Co-Occurring Disorders Treatment
For the Best Possible Chance of Full Recovery, Your Care Should Include:
- Specialists in substance abuse and mental health treatment work together to ensure your mental health and substance abuse needs are met.
- Psychotherapy plays a key role in treating co-occurring disorders, but prescription medication may also be required.
- Therapy that enables the client to make choices is the most reliable and widely used approach.
- In the treatment process, all household members, including partners, spouses, children, and any other members of a household or household members should all be involved regardless of whether they receive individual treatment or take part in family meetings
Co-Occurring Disorders Resources
Receive treatment for co-occurring disorders today.
As the addiction treatment community begins to realize that addiction is itself a mental disorder, the relationship between substance abuse and mental disorders becomes more complicated. The greater treatment community largely lacks a proper understanding of dually diagnosed conditions, so these conditions are still treated separately, or worse–not treated or diagnosed at all. We Level Up TX dual diagnosis treatment centers in We Level Up Florida, California, Texas, New Jersey, Washington are some of the facilities that have professionals trained to help treat co-occurring disorders concurrently. This type of tandem treatment provides some of the best success rates.
Get co-occurring disorders treatment for individuals struggling with substance abuse and mental health disorders. Call us today!
Sources:
[1] Dual Diagnosis – U.S. Department of Health and Human Services National Institutes of Health
[2-5] Co-Occurring Disorders: The Most Popular – https://dualdiagnosis.org/mental-health-and-addiction/
[3] Substance Misuse and Substance use Disorders: Why do they Matter in Healthcare? – National Center for Biotechnology Information
[4] Substance abuse in patients with schizophrenia – National Center for Biotechnology Information, U.S. National Library of Medicine